Alcohol use disorder (AUD) is highly prevalent in the UK adult population, with 4% of people between 16 – 65 years old being alcohol dependant and 24% of adults consuming alcohol in a way that is potentially harmful.
The Chief Medical Officer’s guidelines for both men and women state that in order to keep health risks from alcohol to a low level it is safest not to drink more than 14 units a week on a regular basis.
One unit is 10ml of pure alcohol. Because alcoholic drinks come in different strengths and sizes units are a good way of telling how strong your drink is.
High levels of stigma regarding alcohol use disorder and anxiety about judgment and potential professional consequences should a problem be detected can affect the willingness of an individual to seek help.
Alcohol support through Canopi
Canopi provides a highly confidential, evidence-based service for health and social workers in Wales.
Canopi operates in a climate of trust and openness to avoid feelings of fear and shame and strives to offer an opportunity for all in health and social care to receive appropriate mental health and alcohol misuse support.
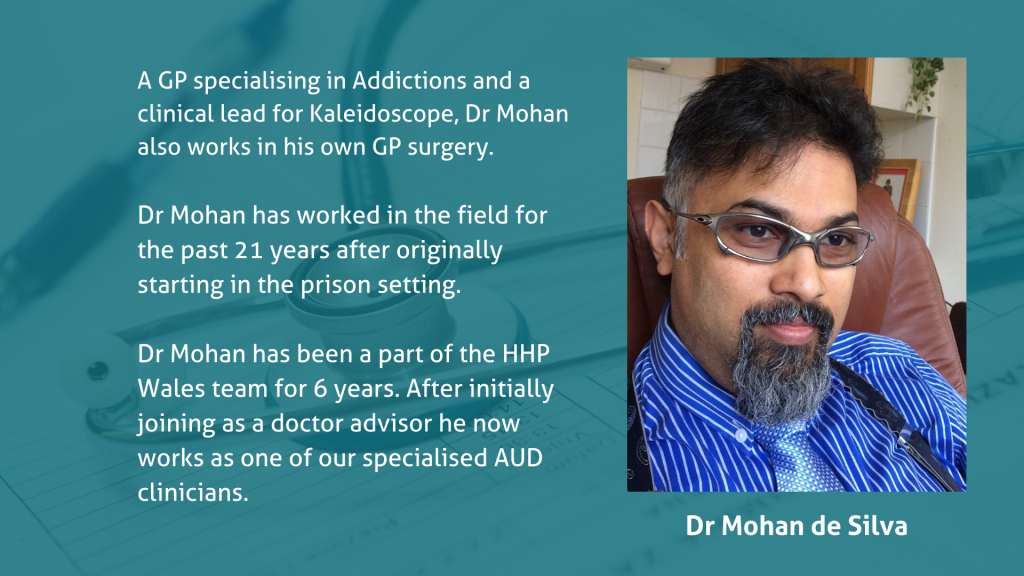
To shed further light on this important service, two members of the Canopi team, Dr Bern Hard and Dr Mohan de Silva, have kindly agreed to discuss the alcohol use disorder service in more detail.

“I think a lot of people worry about confidentiality, stigma and the consequences of disclosing information about alcohol use.
“The principles that underpin our AUD service are insight and cooperation.”
Dr Bern Hard
What is the history of the service?
Dr Mohan:
“The service is an evolvement of the original HHP Wales.
“Prior to the COVID-19 pandemic, Canopi was set up for health care professionals who were doctors working in Wales and the service offered structured cognitive behaviour therapy (CBT) to those who would benefit from mental health support.
“Following the pandemic, access to Canopi services was expanded to all individuals working for NHS Wales. It was also envisaged that due to the circumstances of COVID-19 there would be an increasing number of health care providers with AUD.
“With this in mind, the original Canopi screening questions were expanded to include AUDIT (questions about alcohol consumption and possible alcohol-related problems) to help identify such individuals.”
Could you provide a brief overview of the service?
Dr Bern:
“The AUD pathway is really aimed at exploring alcohol use in greater depth when it has been identified as a possible factor during the initial conversation with the Canopi Doctor Advisor.
“We screen for AUD using a standardised tool called AUDIT.
“This tool can flag up patients whose use of alcohol may be detrimental to their wellbeing in a number of different ways.
“The AUD assessment allows for a detailed discussion about the patient’s current and past relationship with alcohol, and whether this is impacting negatively on them.
“The assessment aims to establish if the alcohol use is hazardous, actually causing harm or if there is any degree of physical dependence – and if so, how severe is this.
“This allows for us to guide patients towards the most effective strategies to manage the problem.
“Non-dependant use can usually be managed by specialist support and guidance, which we can provide with a referral to a CBT therapist with expertise in working with AUD.
“If patients are using alcohol in such a way that they have come to depend physically on it, then it is more appropriate to advise engagement with a specialist service in their local area. We aim to facilitate this next step where needed.”

If someone was considering using the alcohol use disorder service, what would you like them to know?
Dr Bern
“When treating health care providers, we need to always have an eye on the effects that the patient’s own health could have on their ability to treat their patients safely.
“All health care providers have a duty to ensure that their own ill health does not impact negatively in a professional capacity.
“The risk of this occurring is increased if we operate in a culture of fear and secrecy.
We at Canopi accept that health care providers are human. People first. And all people have problems.
“With help and support we can address those problems together, in a way that fosters wellbeing in the health care provider, in the NHS workforce, and in turn, reduces risk to our own patients.
“Confidentiality needs to be balanced with transparency and sharing of information where it is in the best interest of the patient.
“Largely speaking, there is no need to share information outside Canopi where the health care patient has good insight into their own health and is prepared to follow the advice of professionals.
“There are cases where insight is lacking, and we do need to share information in order to protect patient safety, but these are rare, and even then the aim is always to support the health care patient to recover.”

Could you share any insight into the difference you’ve seen the service make to your users?
Dr Mohan
“In most cases, the health care professionals leave with deeper insight and benefit immensely from the extra support they receive from the AUD service.
“My experience is that most instances I have dealt with do not require formal detoxification and I’m reassured by the extra steps that they take with our service.
“While some health care professionals worry about confidentiality, they value the opportunity to talk to someone ‘anonymously’ – I believe this is somewhat easier on the telephone and Canopi give them this confidence.
“I believe the service is an invaluable help to professionals by giving them an opportunity to discuss their problems outside of their employment and giving them a fair amount of confidentiality to discuss their problems openly without being embarrassed.”
Resources
- Canopi referral form
- Canopi self-help resources
- NCMH mental health leaflets

